Menopause is often associated with hot flashes and missed periods, but many women experience significant changes in their genitourinary system—the vagina, vulva, bladder, and urethra—that are less talked about but hugely impactful. These changes are caused by declining estrogen levels and can affect comfort, urinary function, and intimacy.
But the good news is that these symptoms are common and treatable.
What Is the Genitourinary System?
The genitourinary system includes both genital and urinary organs:
- Genital organs: vagina, vulva, cervix, and nearby tissues
- Urinary organs: bladder and urethra
These organs share blood flow, nerves, and the crucial hormone estrogen, which helps keep tissues thick, elastic, lubricated, and resistant to irritation and infection.
How Menopause Affects Your Genitourinary System
During menopause, estrogen production falls sharply. Unlike fluctuating symptoms such as hot flashes, the drop in estrogen causes lasting changes in tissue structure and function. This condition is medically known as Genitourinary Syndrome of Menopause (GSM), impacting between 27% to 82% of postmenopausal women menopause society. Despite how common it is, many women don’t receive the care they need.
As estrogen declines:
- Vaginal walls become thinner and less elastic
- Natural lubrication decreases
- Vaginal pH rises from acidic to more neutral, increasing infection risk
- The bladder and urethra lose support, leading to urinary symptoms
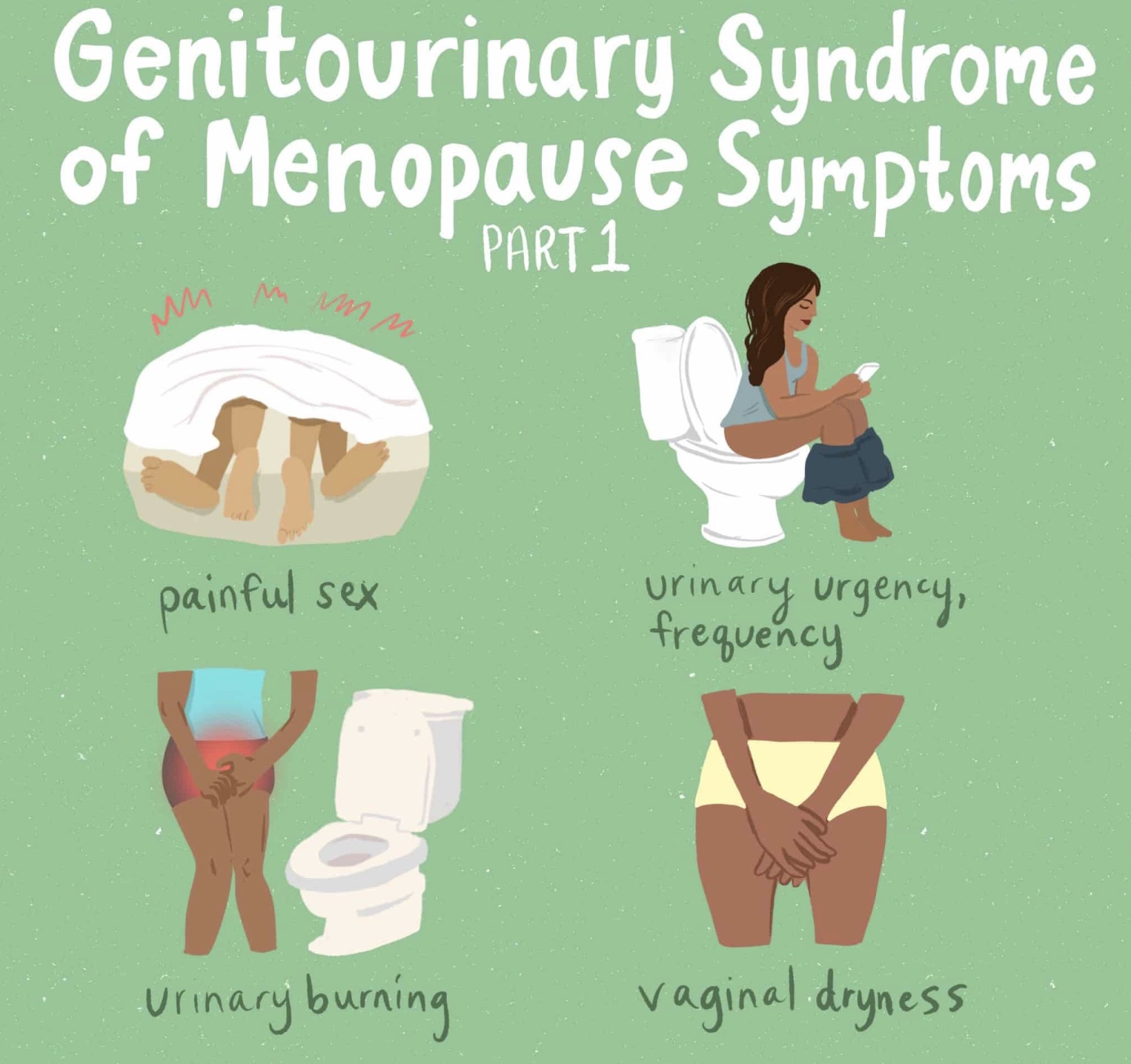
Common Vaginal and Urinary Symptoms
Symptoms often start slowly but can worsen if untreated. They include:
- Vaginal dryness, burning, itching, or irritation
- Soreness or tearing, especially during sex
- Pain or discomfort during intimacy (called dyspareunia)
- Increased need to urinate frequently or urgently
- Burning sensation while urinating without infection
- Recurrent urinary tract infections
- Leaking urine when coughing or exercising (stress incontinence)
These symptoms are caused by physical changes—not by age alone or hygiene issues—so it’s important to address them rather than ignore them.
Everyday Effects and Quality of Life
GSM can quietly disrupt daily life by causing discomfort, reducing sexual enjoyment, and creating fear of bladder accidents. Women might avoid activities such as workouts, travel, or social events. Nighttime trips to the bathroom can disrupt sleep, affecting energy and mood. Over time, these effects can feel isolating but they don’t have to be a permanent part of life.
How to Find Relief and Care
Fortunately, many safe and effective options help restore comfort and function:
- Vaginal moisturizers: Regular use improves long-term tissue hydration
- Lubricants: Provide relief during sex
- Localized vaginal estrogen therapy: Low-dose creams, tablets, or rings rebuild tissue and normalize pH with minimal hormone absorption
- Vaginal DHEA (prasterone): Converts locally into hormones to improve tissue health
- Ospemifene: An oral medication that directly targets vaginal estrogen receptors
- Pelvic floor therapy: Strengthens muscles that support bladder control and pelvic health
- FDA approved radio-frequency devices like EmpowerRF is a non-surgical, multi-technology platform for women’s wellness, using radio-frequency (RF) and Electrical Muscle Stimulation (EMS) to treat issues like pelvic floor weakness, vaginal dryness, urinary incontinence and laxity by tightening tissues, boosting collagen, and strengthening muscles.
Localized estrogen treatments are safe for most women, even those with complex medical histories, but personal evaluation is essential to choose the right approach.
Factors That Can Make Symptoms Worse
Certain conditions can accelerate or worsen genitourinary symptoms:
- Smoking
- Surgical or early menopause
- Chemotherapy or pelvic radiation
- Long-term anti-estrogen medication use
- Lack of sexual activity, which normally helps maintain healthy blood flow
Recognizing these can help guide prevention and treatment choices.
Addressing Genitourinary Symptoms
It’s common for women to believe these symptoms are simply an unavoidable part of aging, or to feel hesitant discussing them. Meanwhile, healthcare providers may concentrate on other health priorities like bone density or cardiovascular risks, leaving genitourinary issues unaddressed unless patients raise the topic. Recognizing and discussing these concerns openly can lead to timely diagnosis and effective treatment, improving overall well-being and quality of life.
If you’re experiencing any of these symptoms, don’t wait. Reach out to a menopause specialist who can tailor treatment to your needs. At MenopauseClinicDE.com, we offer compassionate, expert care to help you regain your confidence.
Related Posts
- A Man’s Practical Guide to Understanding and Supporting His Partner Through Menopause
- Black Box Warning Removed from Menopause Hormone Therapy as FDA Reverses 23-Year Stance